AI-powered remote patient monitoring (RPM) is rapidly reshaping how we care for patients—especially the elderly and those with chronic conditions. By combining artificial intelligence with wearable sensors, healthcare providers can now track patient health in real-time, personalize interventions, and improve clinical outcomes—all without the need for constant in-person visits.
What is AI remote patient monitoring?
Remote patient monitoring AI refers to the integration of artificial intelligence into RPM systems that track and analyze patients’ health data remotely. Traditionally, RPM systems gathered data from blood pressure cuffs, glucose monitors, and other medical devices. But today, AI algorithms can now process this data to detect subtle patterns, predict complications, and alert clinicians in real time.
Instead of manually reviewing large volumes of patient data, healthcare teams can rely on machine learning to prioritize urgent cases, identify health deterioration early, and optimize treatment plans. This is a game-changer for RPM in telehealth, especially in rural areas or underserved communities where access to care is limited.
➲ Discover more about the Benefits of ChatGPT in Telemedicine
The Role of Wearable Sensors in RPM
At the heart of AI-powered RPM are wearable sensors—smartwatches, ECG patches, biosensors, and fitness trackers—that continuously collect data such as heart rate, oxygen saturation, physical activity, sleep patterns, and more.
These devices have become increasingly comfortable, unobtrusive, and reliable. When connected to AI-driven platforms, wearable sensors do more than track—they interpret. For example, an AI model can distinguish between a temporary spike in heart rate caused by exercise versus one caused by arrhythmia. This nuanced understanding is critical for timely intervention.
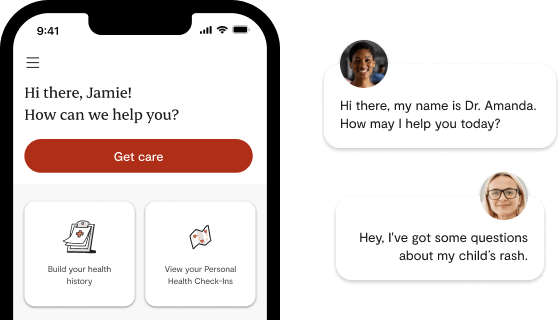
RPM in Telehealth: Beyond Virtual Consultations
While telehealth gained momentum during the COVID-19 pandemic, RPM in telehealth is now proving essential for continuous care. Unlike standard telemedicine, which relies on scheduled video calls, RPM allows for ongoing, real-time monitoring. This continuity bridges the gap between visits and provides clinicians with a fuller picture of the patient’s health.
AI systems can flag early warning signs, such as worsening heart failure or risk of falls, and automatically notify care teams. This proactive approach is especially beneficial for managing chronic diseases like diabetes, hypertension, and COPD—conditions that require frequent monitoring and timely interventions.
Revolutionizing Elder Care Tech
One of the most transformative applications of AI-powered RPM is in elder care tech. Older adults often face multiple health challenges, cognitive decline, and a higher risk of hospitalization. With AI-enabled monitoring tools, caregivers can detect subtle changes in behavior, mobility, or sleep patterns that may indicate underlying health issues.
For example, a decrease in walking speed combined with irregular sleep and heart rate variability might signal early signs of frailty or an impending health crisis. AI can pick up on these trends long before a human caregiver might, allowing for preventive action.
Moreover, integrating these systems with emergency response protocols adds a layer of safety. If a fall is detected, the system can notify caregivers or emergency services immediately—reducing the time it takes to get help.
The Research Behind the Technology
A growing body of research supports the effectiveness of AI-powered RPM. A notable study published on arXiv (arXiv:2301.10009) highlights how machine learning models applied to wearable sensor data can predict health deterioration with impressive accuracy.
These models were trained on datasets collected from various wearable devices, learning to detect health anomalies in real time. Their success points to a future where predictive analytics becomes a standard tool in personalized healthcare.
Challenges and Ethical Considerations
Despite its potential, the adoption of remote patient monitoring AI comes with challenges:
- Data privacy and security: Protecting sensitive health information is paramount.
- Equity of access: Not all patients have access to wearable technology or broadband internet.
- Algorithmic bias: AI systems must be trained on diverse data to avoid biased predictions.
Stakeholders must work together—clinicians, developers, regulators, and patients—to ensure these technologies are safe, equitable, and transparent.
The Future of Healthcare is Intelligent and Remote
The convergence of AI, wearable sensors, RPM in telehealth, and elder care tech signals a paradigm shift in healthcare delivery. These tools don’t just extend care beyond hospital walls—they redefine what care can be.
By empowering clinicians with real-time data and predictive insights, AI-powered RPM is paving the way for more personalized, proactive, and efficient healthcare—especially for the elderly, chronically ill, and those living in remote areas.